Medical Frontier Communicator
Connecting Doctors & Sharing Better
iCardioOncology
▼
1
// Background
Due to the unavoidable influence of extracorporeal circulation, cardiac surgery will cause varying degrees of damage to the patient’s liver, heart, lungs and other organs and the coagulation mechanism, affecting the patient’s prognosis. About 10% of high-risk cardiac surgery patients may have abnormal liver function after receiving CPB, which directly affects the morbidity and mortality of patients, and seriously affects the quality of life of patients. Therefore, timely and effective intervention is required.
Abnormal liver function tests (LFTs) after coronary artery bypass grafting may be due to reduced hepatic blood flow, hypoxia, or pump-induced inflammation. In addition, the severity of liver disease and the degree of abnormal liver function indicators significantly affect the prognosis of cardiac surgery. However, there are few studies on the correlation between preoperative LFT abnormality and prognosis in cardiac surgery patients.
This article investigated the associations between preoperative LFTs and ICU and length of stay, in-hospital mortality, 90-day mortality, and 4-year mortality in cardiac surgery patients without liver disease.
2
// Methods
Adult cardiac patients without liver disease (≥ 18 ) included in the database (The Medical Information Mart for ICU III, MIMIC-III ) age).
The Spearman correlation test was used to analyze the correlation between LFTs and hospital stay and ICU length of stay.
Survival curves were calculated using the Kaplan-Meier method and compared using the log-rank test.
Multivariate logistic regression analysis was used to identify LFTs as an independent prognostic factor for mortality.
3
// Results
Baseline characteristics of the study population
A total of 2565 patients were included in this study, of whom 63 (2.46 %) patients died. There were no significant differences in age, sex or weight between non-survivors and survivors. Non-survivors had lower ALB values (3.8 vs. 3.4, p=0.000), ALT (22 vs. 29, p=0.000), AST (26 vs. 60, p=0.000) and total bilirubin (0.6 vs. 0.7) , p=0.000) is higher. Non-survivors tended to have shorter heights, lower SBP, body temperature, and SpO2 values, higher RR, creatinine, BUN, SAPS II, and SOFA scores, and a history of congestive heart failure, hypertension, chronic lung disease, and renal failure.
The prognostic significance of liver function indexes in cardiac surgery patients without liver disease
Spearman’s rank correlation test was used to explore the relationship between liver function indexes and hospitalization time and ICU length of stay in cardiac surgery patients without liver disease. The results are shown in Table 2. ALB was significantly negatively correlated with ICU and hospital stay, and ALT, AST, and total bilirubin were significantly positively correlated with ICU and hospital stay.
Secondly, to explore the correlation between liver function indexes and in-hospital mortality in patients without liver disease undergoing cardiac surgery (Table 3). ALB, ALT, AST, and total bilirubin quartiles were significantly associated with in-hospital mortality. For ALB, the first quartile had higher hospital mortality; for ALT, AST, and total bilirubin, the fourth quartile had higher hospital mortality. Similar trends were observed when grouping by clinically normal values.
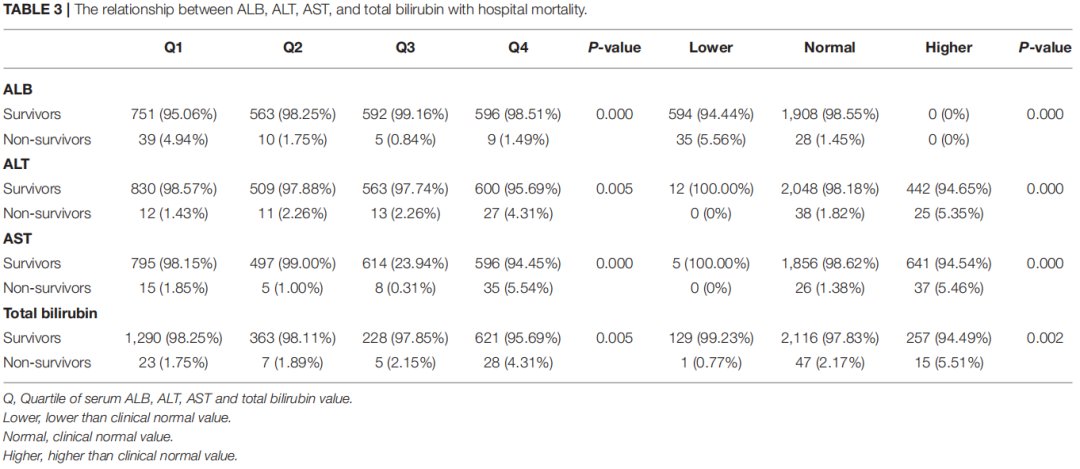
Then, the association of liver function indexes with 90-day mortality in cardiac surgery patients without liver disease was investigated (Table 4). For ALB, higher 90-day mortality was observed in the first quartile; for ALT and AST, higher 90-day mortality was observed in the fourth quartile; total bilirubin On the other hand, the 90-day mortality in the third and fourth quartiles was higher than that in the first and second quartiles (p=0.000). At the same time, grouping by clinical normal values showed different trends than grouping by quartile: for ALB and AST, 90-day mortality was higher in the lower and higher value groups; for total bilirubin, the values were higher The high group had a higher 90-day mortality rate.
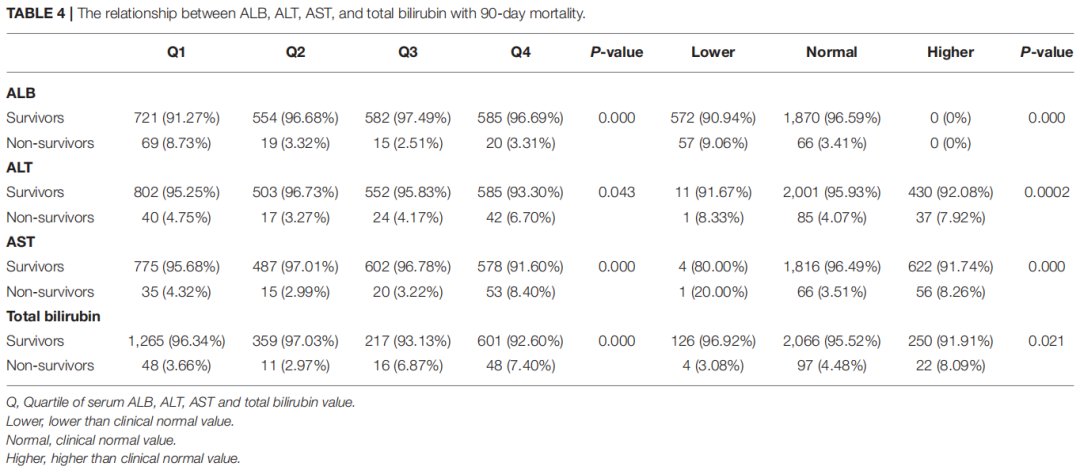
For 4-year mortality, only CareVue patients with at least 4 years of follow-up were analyzed (Table 5). ALB had higher 4-year mortality in the first quartile and below-normal groups (all p=0.000). For AST, higher 4-year mortality was observed in the first and fourth quartile groups (p=0.023) and in the below-normal and above-normal groups (p=0.007). For total bilirubin, 4-year mortality was higher in the third and fourth quartiles and below-normal and above-normal (all p=0.000).

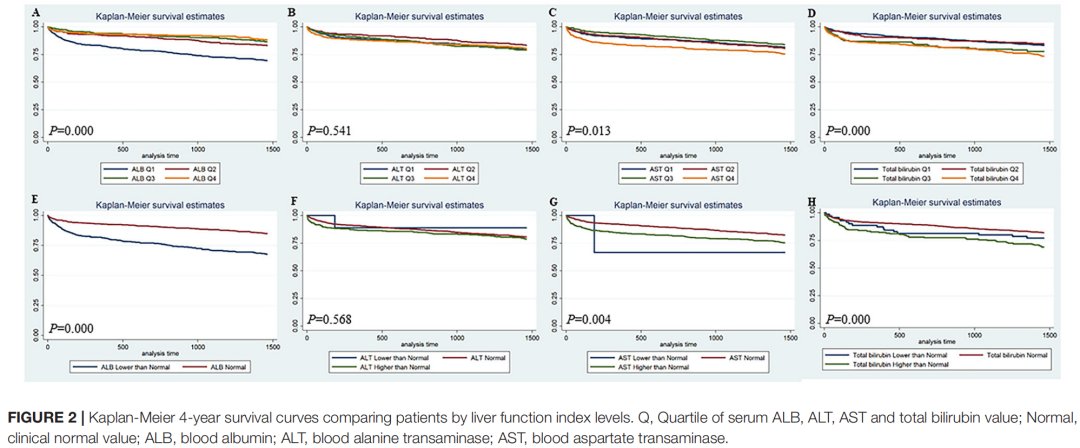
The Kaplan-Meier survival curves of the patients compared with the liver function indexes are shown in Figure 1 and Figure 2. The results showed the lowest 90-day survival in the first quartile of ALB and the fourth quartile of ALT, AST, and total bilirubin (all p<0.05). Patients with lower ALB, lower ALT/AST and higher ALT/AST and higher total bilirubin had lower 90-day survival (all p<0.05). In addition, 4-year survival was lower in the first quartile of ALB, the fourth quartile of AST, and the third quartile of total bilirubin (all p<0.05), while ALT four There were no significant differences in quantile values.

Univariate logistic regression analysis (Table 6). ALB was associated with hospital mortality, 90-day mortality, and 4-year mortality. ALT Associated with hospital mortality and 90-day mortality, but not 4-year mortality. AST was associated with hospital and 90-day mortality, but not 4-year mortality. Total bilirubin was associated with hospital mortality, 90-day mortality It was associated with 4-year mortality.
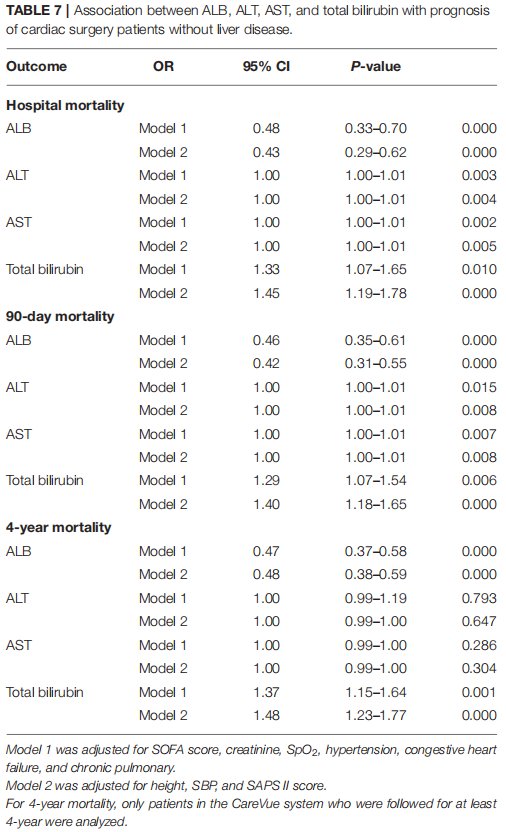
The multivariate statistical analysis results are shown in Table 7. Model 1 adjusted for SOFA score, creatinine, SpO2, hypertension, congestive heart failure and chronic lung disease. Model 2 further adjusted for height , SBP and SAPS II score. ALB was associated with hospital mortality, 90-day mortality, and 4-year mortality in both models. ALT was associated with hospital mortality and 90-day mortality in both models, but was associated with 4-year mortality No. AST was associated with hospital mortality and 90-day mortality in both models, but not 4-year mortality. Total bilirubin was associated with hospital mortality, 90-day mortality, and 4-year mortality in both models.
4
// Summary
exists between the heart and liver Complex pathophysiological interactions. Therefore, the pathological changes of one organ system can cause structural and functional abnormalities of other organ systems. Liver function damage is one of the serious complications of cardiopulmonary bypass surgery. Blood loss and postoperative low cardiac output, etc. Comprehensive liver function assessment is of great significance for determining the liver function status of patients and guiding clinical treatment.
The results of this study showed that ALB, AST, ALT Abnormal total bilirubin is associated with ICU and length of stay, in-hospital mortality, 90-day and 4-year mortality in cardiac surgery patients without liver disease. Abnormal ALB, AST, ALT and total bilirubin are associated with hospital mortality and 90-day mortality However, only ALB and total bilirubin were independent risk factors for 4-year mortality. This study suggested that abnormal preoperative LFTs were associated with short-term and long-term prognosis in patients without liver disease after cardiac surgery.
Serum ALB represents the synthetic function of the liver and is an indicator for evaluating the severity of liver cirrhosis and judging prognosis. Low serum ALB concentration or hypoalbuminemia is generally used as a predictor after cardiovascular surgery. The latter indicators may be caused by congestive heart failure or chronic hepatic insufficiency. In the present study, low preoperative serum ALB was significantly associated with short- and long-term outcomes in cardiac surgery patients without liver disease and could be an independent risk factor for death. ALB levels in non-survivors were significantly lower than in survivors, which may indicate that when ALB levels are lower than normal, the risk of death increases for patients. Therefore, preoperative nutritional supplementation and correction of hypoalbuminemia can benefit cardiac patients before cardiac surgery and avoid possible adverse effects after surgery.
Elevated serum total bilirubin can be caused by hemolysis, decreased hepatic perfusion, chronically low cardiac output, or liver cell dysfunction caused by right heart failure and hepatic congestion. Preoperative serum bilirubin level is an independent risk factor for cardiac surgery in patients with liver cirrhosis. The results of this study suggest that preoperative high serum total bilirubin may serve as an independent risk factor for short- and long-term prognosis in patients without liver disease undergoing cardiac surgery. Elevated serum total bilirubin in cardiac surgery patients without liver disease may be due to hepatic hypoperfusion and/or hepatic congestion. In this setting, optimal preoperative treatment of congestive heart failure can reduce preoperative serum total bilirubin levels. But this conjecture needs more research to confirm.
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are markers that reflect liver cell damage and can be released into the blood immediately after heart failure causes liver damage. This study is consistent with previous findings. Among cardiac surgery patients without liver disease but without 4-year mortality, ALT and AST were independent risk factors for hospital mortality and 90-day mortality.
In conclusion, this study demonstrated that abnormal LFTs were significantly associated with ICU and hospital stay in cardiac surgery patients without liver disease. Abnormal LFTs are associated with higher hospital mortality, 90-day mortality, 4-year mortality, and lower 90-day and 4-year survival rates. LFTs can be used as independent predictors of hospitalization, 90-day and 4-year mortality in cardiac patients without liver disease.
As a single-center retrospective study, this study also has all the limitations of a retrospective observational study and therefore needs to be further confirmed in a larger multicenter cohort or randomized controlled trial. In addition, large differences in the number of survivors and non-survivors may have contributed to the study’s bias.
【References】
[1] Shang L, Ao Y, Lv L, Lv L, Zhang Y, Hou J, Yao J, Wu Z. Preoperative Liver Function Test Abnormalities Were Associated With Short-Term and Long-Term Prognosis in Cardiac Surgery Patients Without Liver Disease. Front Cardiovasc Med. 2021 Nov 1;8:772430. doi: 10.3389/fcvm.2021.772430. PMID: 34790710; PMCID: PMC8591306.
[2] Xu Wanglan, Fang Qiang. Perioperative changes of liver function and related risk factors in patients undergoing cardiopulmonary bypass surgery[J].Chinese Journal of Circulation,2015,30(11):1086-1089.
p>
[3] Li Xuanfa, Tang Jingying, Xu Zhixin, Liu Lili, Wei Xuemei. Study on the expression level of liver function in patients with cardiopulmonary bypass and the intervention mechanism of adenosylmethionine [J]. Advances in Modern Biomedicine, 2019,19 (08):1529-1532.DOI:10.13241/j.cnki.pmb.2019.08.029.
Content organization: Leadman Sales Department Graphic Design: Sandu Medical CtrlZ Typesetting Editor: Sandu Medical Simin
Editor-in-Chief: Third Degree Medical May