Femoral head necrosis is a pathological evolution process, that is, the repair reaction of necrotic bone resorption and new bone ingrowth immediately after necrosis. With the progress of imperfect repair, the local mechanical properties change, and under the action of stress Microfractures (ie, collapse of the head).
The author of this article: Zhou Chi
The process of such collapse-repair continues, resulting in collapse and deformation of the articular surface of the femoral head, degeneration of articular cartilage, with or without hip subluxation, disfunction.
At present, the trend of rejuvenation of femoral head necrosis is increasing year by year. However, in the early stage after femoral head necrosis, there are no symptoms or only mild discomfort (soreness of the hip, etc.), and there are almost no abnormal changes in X-ray and CT examinations.
Collapse occurred in the mid-term, and at the same time showed obvious pain symptoms. At this stage, osteonecrosis of the femur has gone through a long period of time (as little as half a year, as much as 2-3 years, as shown in Figures 1 and 2). Don’t think that it is still in the early stage of necrosis of the femoral head, you are lucky, misbelieve various rumors, and think that you can use remedies to change the condition and magically cure it, this is impossible!
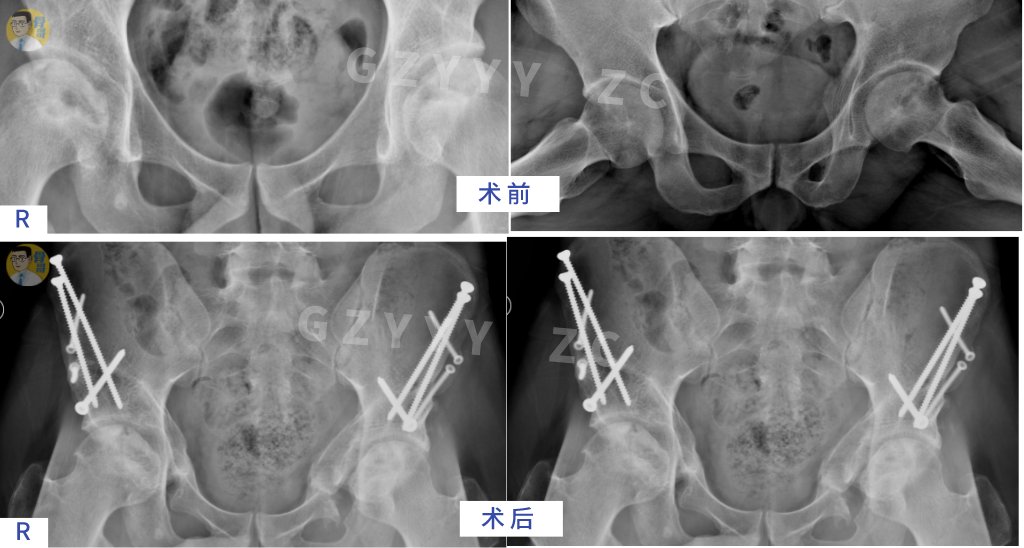
Collapse is the key point for the success or failure of hip preservation in femoral head necrosis. Before and early post-collapse (ie: peri-collapse period, within 1 year after collapse, collapse ≤ 2mm) is also the treatment of hip preservation for femoral head necrosis. Last chance.
Patient Cases
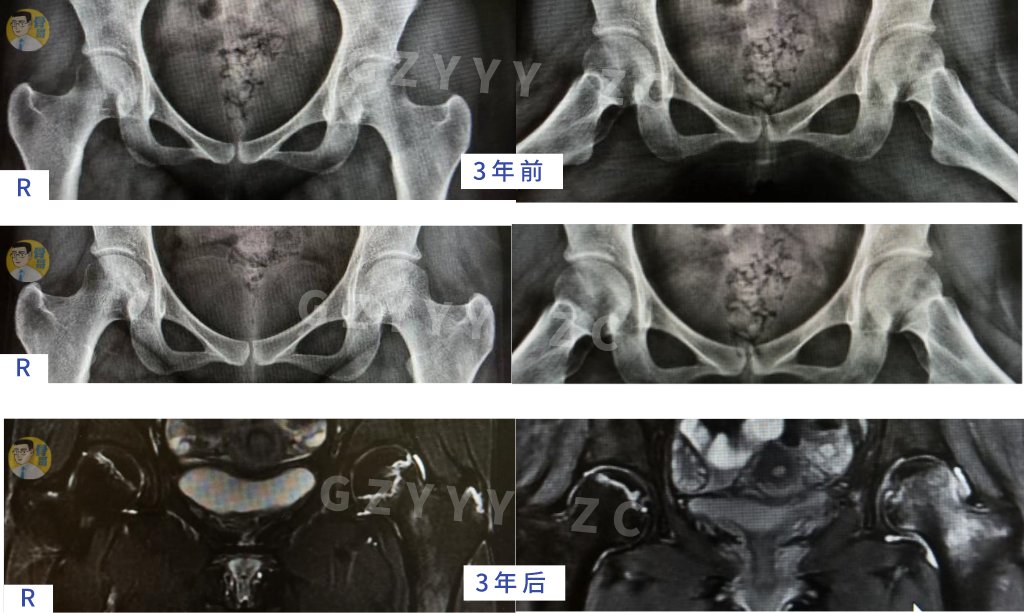
Case 1: Female, 26 years old, steroid-induced femoral head necrosis (double 3 years later, there were no obvious symptoms (only occasional soreness and sleepiness in the hip). After 3 years, the pain in the left hip increased instantly, and the patient was limping. The X-ray film still showed no obvious collapse change, and the MRI showed a clear rupture zone in the femoral head.
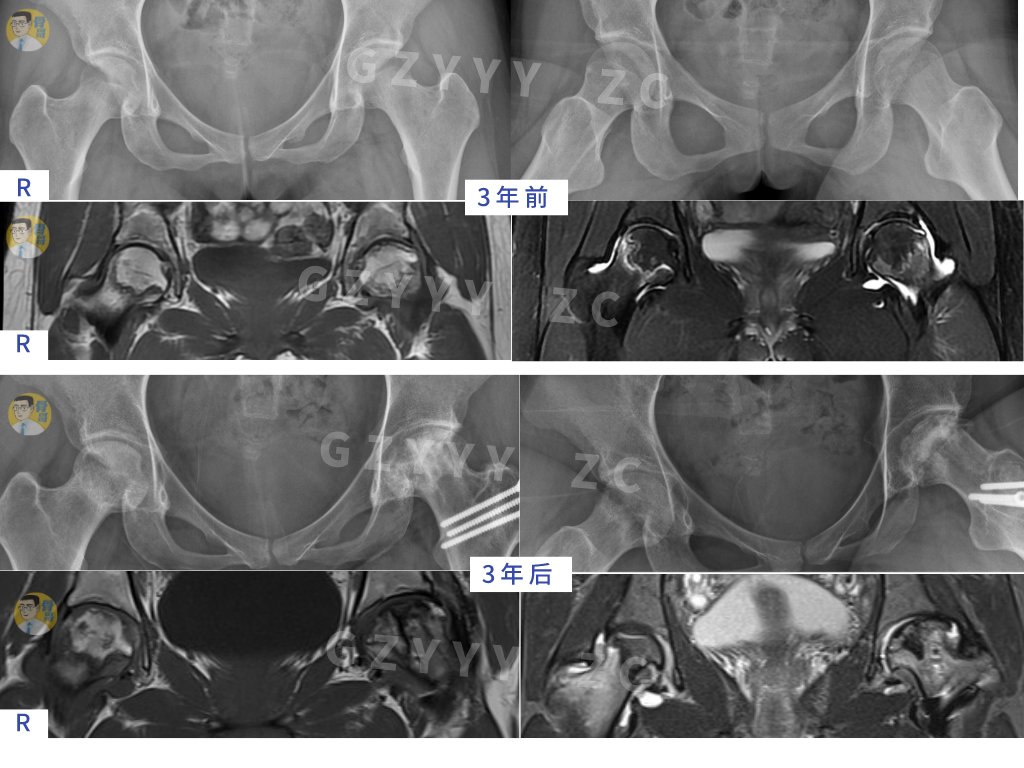
Case 2: Female, 23 years old, hormonal femoral head necrosis (bilateral), left side collapse, right side There was no collapse and no obvious symptoms within 3 years (only occasional soreness in the hip). After 3 years, the pain in the right hip increased instantaneously, and the patient was limping.
Therefore, for high-risk groups of femoral head necrosis, such as long-term alcoholism, hormone use, or history of hip trauma, it is necessary to conduct a magnetic resonance (MRI) examination in time under the guidance of a specialist. .
Confirm whether there is necrosis of the femoral head and the type of necrosis, and conduct early diagnosis and accurate comprehensive evaluation to determine which hip preservation scheme is suitable, rather than simply relying on the early, middle, and late stages of femoral head necrosis. Define your hip protection plan.
For small-scale necrosis that deviates from the medial side of the femoral head, oral Chinese patent medicine treatment and functional exercise can be used to protect the hip.
For the type of necrosis involving the anterolateral wall of the femoral head in a large area, the hip-preserving surgery plan is tailored.
Don’t wait until the large-scale collapse, the pain is unbearable, and the function is severely limited before thinking of hip preservation by surgery, losing the last chance of “hip preservation”.
In addition, even for hip preservation, different types of surgical plans are used. Choosing the right hip preservation plan for you is related to the final outcome of the development of femoral head necrosis. Don’t miss the opportunity.
Whether it is surgical hip preservation or drug hip preservation, the choice of indications is very important. In the stable repair period, even if there are occasional mild pain symptoms, surgical intervention is generally not required.
Especially young patients should have full confidence in hip preservation for femoral head necrosis, and accept standardized and professional systemic treatment. It should not be delayed again and again, let alone blindly confuse femoral head necrosis with anti-osteoporosis treatment, and simply take it. Calcium tablets, I thought they could heal themselves!
Precision hip preservation program
1. Non-surgical Chinese medicine comprehensive hip preservation (eg: male, 42 years old, bilateral femoral head necrosis and alcohol)
2. Minimally invasive surgery for hip preservation (removal of lesions in the femoral head and compression of bone graft + allograft fibular support, example: male, 39 years old, steroid-induced femoral head necrosis, 15 years after operation, good function, no pain)
3. Debridement of lesions in the femoral head and bone grafting + autologous iliac bone support (male, 32 years old, bilateral femoral head necrosis and alcohol, good function after 3-year follow-up, no discomfort)
< img class="content_title" height="300" layout="responsive" sizes="(min-width: 320px) 320px, 100vw" src="https://p0.ssl.img.360kuai.com/t01f05eb0c9bb9b8606.jpg" width="600">
4. Rotational osteotomy of the base of the femoral neck (male, 36 years old, bilateral femoral head necrosis hormone, the weight-bearing area of the femoral head was completely normal after surgery Bone, necrotic area is repaired spontaneously and stably)

5. Periacetabular Rotation Osteotomy (PAO) to improve head The acetabular inclusion relationship promotes the plastic repair of the femoral head (male, 32 years old, bilateral femoral head necrosis hormone, good recovery 1 year after surgery, necrotic repair, normal function, no pain)
Dr. Zhou Chi suggested that the choice of hip preservation for femoral head necrosis largely depends on the location and volume of the necrotic area, combined with the repair stage at that time, rather than Time, it is not that the hip preservation of femoral head necrosis surgery is definitely better than non-surgery, suitable for self- Your own is the best!
Cooperative email: jdh-hezuo@jd.com
The author of this article: Zhou Chi, The First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine
Responsible editor: Guo Haiyan
p>