This article is reproduced from: People’s Daily Online
People’s Daily Online, Jinan, April 25th. Recently, Mr. Wang from Shandong was unfortunately injured by about 2 tons of steel plate weight in the abdomen and pelvis, and he was rushed to the hospital. The hospital carried out a life-and-death rescue, and was successfully treated after a half-body amputation. At present, Mr. Wang’s condition is stable and is undergoing further treatment and recovery. According to official literature search, this case is the first in the world.
On the afternoon of February 28, 45-year-old Mr. Wang was smashed into his abdomen and pelvis by a weight of about 2 tons of steel plate. He was transferred to the emergency department of Qilu Hospital of Shandong University 3 hours after the injury. On admission, his blood pressure was 97/50 mmHg, heart rate was 138 beats/min, respiration was 28 beats/min, SPO was 2100%, arterial blood gas pH was 7.21, and Lac was 7.9 mmol/L.
Mr. Wang suffered from acute pelvic fracture and massive hemorrhage due to abdominal and pelvic crush injury, extensive tearing of mesentery and small bowel and colon rupture and massive hemorrhage combined with traumatic abdominal aortic injury, followed by acute abdominal aortic occlusion, resulting in lumbar 5 plane The following include severe ischemic necrosis of pelvic bone structure and muscle, skin and soft tissue, acute renal failure due to absorption of toxins into the blood, and life is at stake.
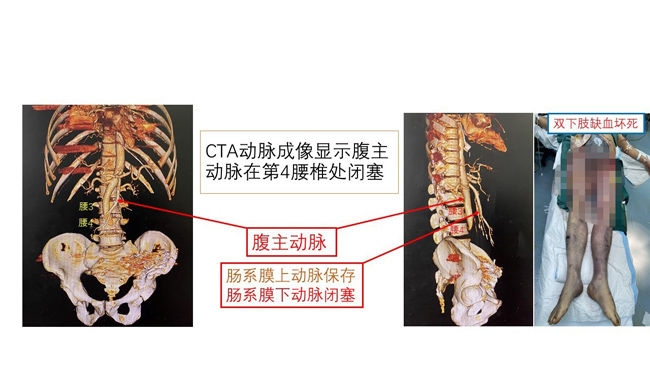
CTA arterial imaging showed that the patient’s abdominal aorta was completely occluded below the L4 vertebral body, and both lower extremities were completely necrotic. Photo courtesy of Qilu Hospital of Shandong University.
The situation is critical! The doctor on duty decisively gave fluid resuscitation, performed massive blood transfusion and re-examination of CT, and quickly activated the green channel for trauma treatment, and urgently contacted the operating room and anesthesiology department to prepare for the operation.
The attending physician quickly transferred the patient to the operating room, performed emergency radiological intervention consultation for angiographic embolization, and reported to Sang Xiguang, the director of emergency surgery.
CT found that Mr. Wang’s ascites, pneumoperitoneum, and retroperitoneal hematoma suggested rupture of abdominal organs, and severe displacement of the pelvic and acetabular fractures suggested pelvic instability and active bleeding. Blood continued to pour out from the pelvic external fixator nail holes, and the hemoglobin continued to decline. The surgical team actively transfused blood and fluids to rescue the patient, and at the same time called for instructions to do iliac arteriography embolization to stop bleeding in the interventional surgery room.
After arriving in the operating room, Sang Xiguang inspected the patient, studied and judged the condition, formulated an emergency surgery plan, and contacted the blood transfusion department to give a lot of blood support.
In critical condition! The patient’s vital signs were extremely unstable, the bleeding was rapid, and the blood pressure dropped rapidly; the lower abdomen was incised and tamped to stop the bleeding, only the skin and subcutaneous tissue were found in the abdominal wall, and the abdominal wall muscles were torn and absent, and the pelvic wall of the left iliac fossa was severely contused and massive bleeding; extensive mesentery Tears, active bleeding in the form of jets, partial necrosis of the small intestine, rupture of the sigmoid colon near the peritoneal reflexion; obvious bleeding in the retroperitoneal laceration, and the formation of a retroperitoneal hematoma…
Therefore, a team of surgeons performed a , Anesthesiologists team, interventional doctors and nurses struggling to rescue patients with traumatic hemorrhagic shock “battle” started.
The trauma treatment team performed necrotic small bowel resection, proximal fistula, necrotic colectomy and sigmoid colon end-to-side anastomosis, abdominal cavity and pelvic gauze packing to stop bleeding. Red blood cells, plasma, platelets, etc. are transfused during the operation. With the tacit cooperation of the medical staff, the operation was successfully completed. After the patient’s vital signs were stable, he was then returned to the emergency surgical intensive care unit with endotracheal intubation.
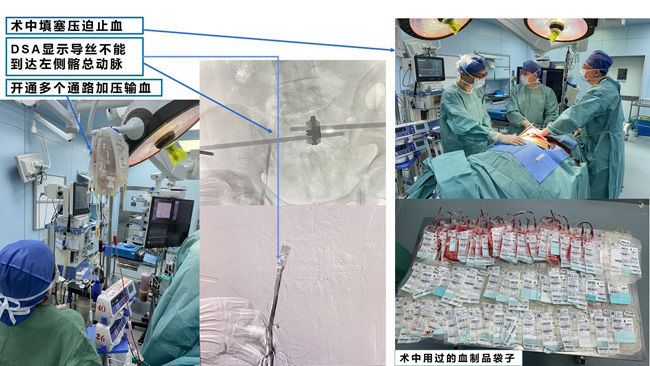
The intraoperative team of surgeons, anesthesiologists, interventionists and nurses worked hard to rescue patients with traumatic hemorrhagic shock. Photo courtesy of Qilu Hospital of Shandong University.
On March 1, the first day after the operation, the patient still had low blood pressure, fast heart rate, etc., and continued to transfuse red blood cells, plasma, platelets, etc. Factor VII (Nooch), the condition gradually stabilized.
Unfortunately, Mr. Wang had acute occlusion of the lower abdominal aorta, which was confirmed by vascular CTA, resulting in extensive tissue ischemic necrosis in the pelvis, hip, and both lower extremities below the waist 5, absorption of toxins into the blood, and renal failure. The functional failure continued to aggravate, seriously affecting the patient’s life, and the skin below the ischemic site was icy-cold, piebald, and completely necrotic.
After the first multidisciplinary consultation of the whole hospital, the emergency surgery organization decided to perform bilateral hip joint amputation first to try to save the pelvis.
On March 4, the trauma treatment team performed bilateral hip amputation, and the wound was suctioned with negative pressure to reduce the absorption of toxins.
After the operation, the wound tissue continued to be necrotic and rancid. On March 7, the hospital again organized a multidisciplinary consultation of the whole hospital. After discussion, it was decided to perform half-body amputation and pelvic amputation.
On March 8, the trauma treatment team first performed residual colostomy and debridement of the pelvic stump.
With the assistance of the urological team, the trauma treatment team performed a half-body amputation through the lumbar 5-sacral 1 + bilateral ureterostomy + wound debridement and negative pressure suction on March 11. The patient’s infection status improved, and renal function gradually recovered under continuous CRRT therapy.
On April 22, with the strong support of Dean Professor Chen Yuguo, the third multidisciplinary MDT case discussion in the whole hospital was held. Ureterostomy leakage, residual large wound cavity and small part of wound necrosis, infection and purulence, fever, increased inflammatory indexes and nutritional support are studied to formulate the next treatment plan.

Multidisciplinary MDT in the whole hospital, including anesthesiology, intensive care, blood transfusion, burns, plastic surgery, and vascular surgery Wait, discuss treatment options. Photo courtesy of Qilu Hospital of Shandong University.
Professor Sang Xiguang from the Emergency Surgery Department of Qilu Hospital of Shandong University successfully treated Mr. Wang with a half-body amputation. He is currently in stable condition and is undergoing further treatment and recovery.
“This is another miracle of life created by the emergency department of our hospital after the successful treatment of a rare penetrating steel bar in 2016.” Professor Chen Yuguo said. (Song Cui, Su Yuxing, Cui Ziang)