One. Causes of PICC catheter blockage
1. External mechanical reasons, such as tight sutures at the catheter puncture site, kinked/pinched catheter, or needleless connector blockage.
2. Depending on the type of drug or solution infused, there is visible precipitation on the catheter or infusion set.
3. Blood is visible in the catheter or attached device, and blood cannot be withdrawn.
4. Internal mechanical causes: such as clip syndrome, secondary catheter ectopic or catheter-related venous thrombosis.
2. Recanalization method for blocked tube
When the venous catheter is blocked, the cause of the blockage should be analyzed, and normal saline should not be forcibly injected.
1. Mechanical blockage
Check the external factors and the patient’s position. If the catheter is twisted and discounted, the blockage can be lifted after the twist and discount is lifted.
2. Non-thrombotic blockage
It is mainly drug-induced blockage. Check the patient’s medication records. If the blockage is suspected to be caused by drug precipitation or lipid residue, consult with the pharmacist to formulate appropriate treatment measure. For the precipitation caused by the drug, it can be adjusted with antagonists (sodium bicarbonate, hydrochloric acid) to restore the precipitate to a dissolved state; or use 0.1mol/L hydrochloric acid to remove the precipitation of incompatible drugs; use 70% ethanol to remove the fat emulsion deposit , thereby restoring duct patency.
3. Thrombotic blockage
Mainly due to increased blood viscosity caused by diseases, such as acute inflammation, malignant tumor, etc.; blood reflux, due to increased superior vena cava pressure, Such as: severe coughing, excessive force or excessive activity of the arm on the side of the catheter, excessive force, and forceful defecation, etc., the pressure in the chest cavity is too large, resulting in blood reflux; after blood collection or blood product infusion, the catheter is not completely flushed, and the blood is in the channel. Due to the formation of blood clot or thrombus in the lumen, the recanalization method of catheter blockage is as follows:
① The operator removes the infusion connector by withdrawing and squeezing, and disinfects the interface with 75% alcohol, and the connection is not less than Withdraw the 10ml syringe, wear sterile gloves, squeeze the catheter by hand from the catheter connector end while withdrawing, and squeeze while pulling, the broken blood clot can be withdrawn to the syringe, and repeat the operation. until the catheter is unobstructed. Pay attention to the withdrawal strength to avoid excessive negative pressure. It is advisable not to damage the catheter. After the catheter is unobstructed, do not inject blood clots in the syringe into the body, and replace the normal saline to flush the tube.
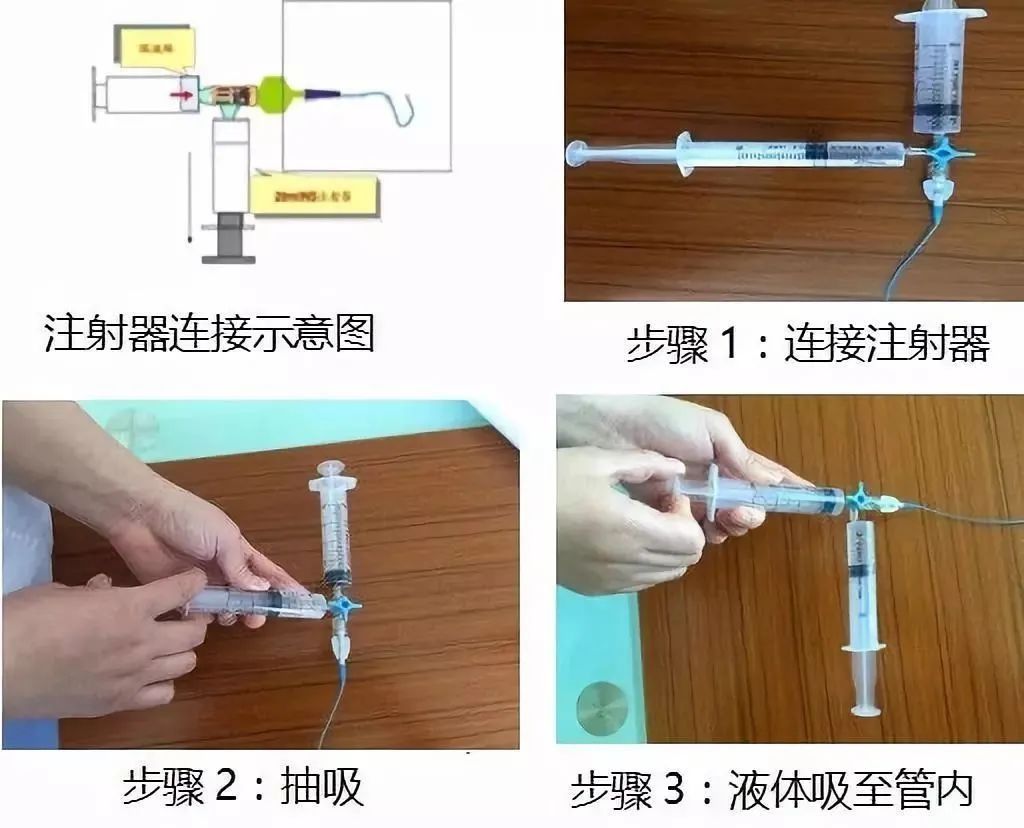
②Intermittent thrombolysis with urokinase This is the most commonly used recanalization method in clinical practice. Urokinase can directly convert inactive plasminogen into active plasmin, hydrolyze the fibrin that forms the thrombus, and exert a thrombolytic effect. In addition, urokinase can also increase the activity of vascular ADP enzyme, inhibit ADP-induced platelet aggregation, and prevent thrombosis. Its main adverse reaction is spontaneous bleeding. Therefore, it is only suitable for patients with normal coagulation mechanism, and patients with suspected bleeding tendency should be used with caution. or disabled. The specific operation method is: take 100,000 units of urokinase and add 20ml of 0.9% normal saline to dissolve, and use a syringe of no less than 10ml to draw 5ml of diluent for use. The operator strictly operates aseptically, puts the patient’s arm below the level of the heart, removes the infusion connector, disinfects it with 75% alcohol cotton, and connects the tee, so that the tee is in a closed state; the connection on the side of the tee is not less than 10ml syringe. The other interface of the tee (that is, in the same line with the catheter) is connected to the syringe that has pumped the liquid medicine, close the tee, open the tee at one end of the empty syringe, withdraw it, and evacuate the PICC catheter into a vacuum, so that a negative pressure is formed in the catheter. pressure, close the tee port; at the same time, open the tee port of the syringe with the urokinase solution, the drug solution enters the catheter using negative pressure, closes the channel between the tee and the catheter, wait for the urokinase solution and the thrombus to be fully mixed, and retain the drug solution After 20 minutes, withdraw once and repeat several times until the catheter is recanalized.
③Heparin saline thrombolysis method When the PICC tube is partially blocked (the fluid can be infused, but the blood cannot be withdrawn), first use heparin The solution is recanalized with heparin saline with a concentration of 100 U/ml for thrombolysis. The specific operation method is the same as that of the urokinase thrombolysis method. Thrombolytic therapy with urokinase was given.
④The method of cutting the end of the tube This method is suitable for the case where a red thrombus can be seen at the end of the catheter, but the rest of the catheter is not blocked, or the patient cannot take thrombolytic methods such as urokinase and heparin or use this method. Use when thrombolysis is ineffective. Specific operation method: remove the dressing, wear sterile gloves, routinely disinfect the puncture site and surrounding skin, pull out the catheter by 0.5-1cm, cut the tube above the thrombus, and try to aspirate and flush the tube each time until it is recanalized. After success, 3-5 ml of blood was withdrawn and discarded, and the tube was sealed with normal saline.
⑤Other methods of systemic thrombolysis or phlebotomy and thrombectomy are suitable for catheter blockage caused by thrombophlebitis. After thrombolysis with urokinase, it cannot be recanalized or the thrombus falls off and causes embolism in other parts. Perform systemic thrombolysis, that is, establish a channel in other peripheral veins for systemic thrombolysis; if thrombolysis is unsuccessful, phlebotomy and embolectomy can be determined according to the condition and lesion site.
Source: Nursing Wellness Station