Recently, the medical staff of Guangxi Chest Hospital (Guangxi Fourth People’s Hospital) worked closely together to successfully perform a difficult bronchoscopic foreign body removal operation for a patient. The patient who was mistakenly put into the “qi” way by the duck claw bone is recovering well and is about to be discharged from the hospital.
Three months ago, the patient developed cough and sputum. Because it was mistaken for a common cold, he was treated in a community hospital, but there was no improvement.
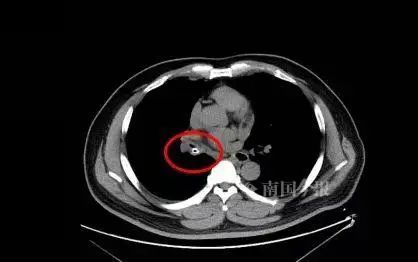
In mid-May, the patient went to Guangxi Chest Hospital for treatment. After completion of CT and various examinations, the patient was diagnosed with a right middle bronchus foreign body with infection in the middle and lower lobes of the right lung. The doctor believes that the patient’s repeated coughing is likely caused by a foreign body choked into the trachea.
The patient told the doctor that he had been intoxicated 3 months ago. At that time, I had eaten duck feet, and it is possible that the bones of the duck feet choked into the trachea. After the cause and diagnosis were clarified, the Department of Respiratory Medicine of the hospital immediately arranged for the patient to undergo painless fiberoptic bronchoscopy and perform tracheal foreign body removal.
The doctor saw under the microscope that the foreign body had completely filled the patient’s tracheal cavity, the patient’s mucosa was congested and swollen, and the foreign body was incarcerated in the bronchial tube wall. In addition, under anesthesia, the patient’s blood oxygen saturation will drop rapidly, which cannot support the patient to complete the operation.

After the doctor in charge reported the patient’s condition to Director Huang Dayong, Huang Dayong believed that in view of the patient’s endoscopic surgery The risk is high and the surgical plan needs to be redesigned. Therefore, the hospital conducted a multidisciplinary consultation.
Experts from the Department of Respiratory Medicine, Department of Thoracic and Cardiovascular Surgery, Department of Imaging, and Department of Surgical Anesthesiology in the hospital agreed that the CT image of the patient’s chest showed that the right middle bronchus had a foreign body incarcerated, the foreign body was long, and it was indwelled. The time in the trachea is long, the inflammatory reaction is severe, and the foreign body is rashly removed under conventional bronchoscopy, and the risk of major bleeding is extremely high. Endoscopic right middle tracheal foreign body removal can be performed in the operating room with endotracheal intubation. If major bleeding occurs, tracheal balloon occlusion is performed immediately, and thoracotomy is performed for foreign body removal, or right middle and lower lobectomy.
After taking into account the patient’s medical history and expert opinion, the patient was transferred to thoracic and cardiac surgery.
On May 25, after multidisciplinary collaboration, after anesthesia and intubation in the anesthesiology department of the hospital, Director Huang Dayong used a bronchoscope to successfully remove a 3-centimeter long bone for the patient, which was successfully opened for the patient. a “channel of life”. At the same time, the patient was prevented from undergoing thoracotomy, and the middle and lower lobes of the right lung were preserved for him.

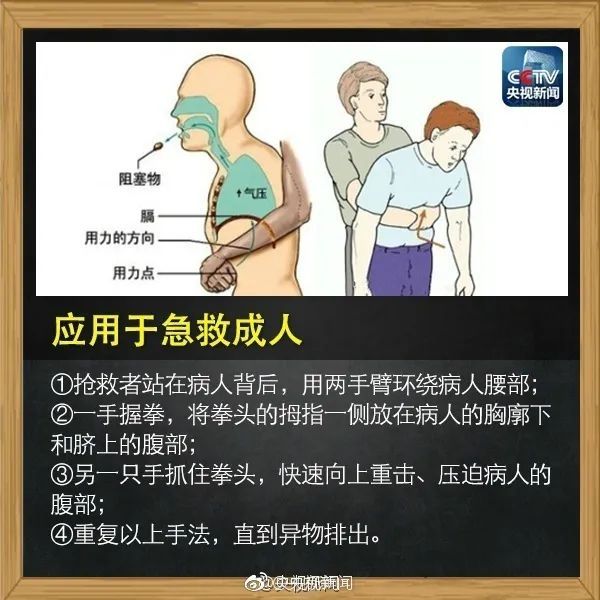
According to Director Huang Dayong, foreign bodies in the trachea mostly occur in children, the elderly and infirm, and patients with craniocerebral accidents In healthy adults, it also occurs occasionally, and the incidence is higher when intoxicated. When the foreign body blocks the trachea seriously, it will cause suffocation, and the Heimlich method should be used for first aid, or the hospital should be quickly sent to the hospital for treatment.
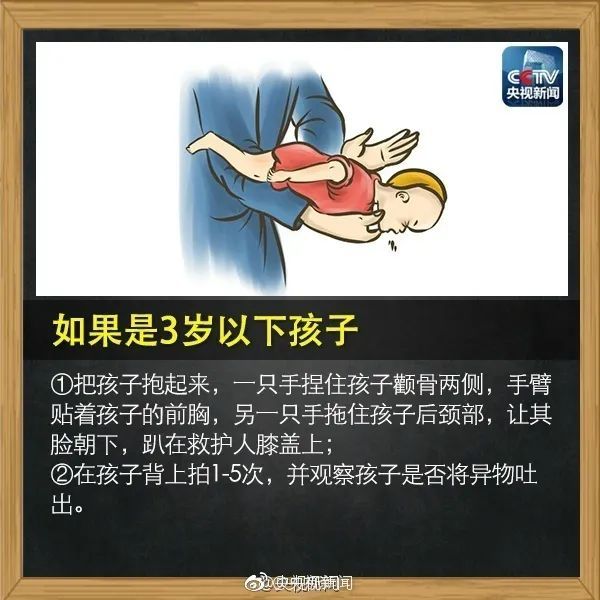
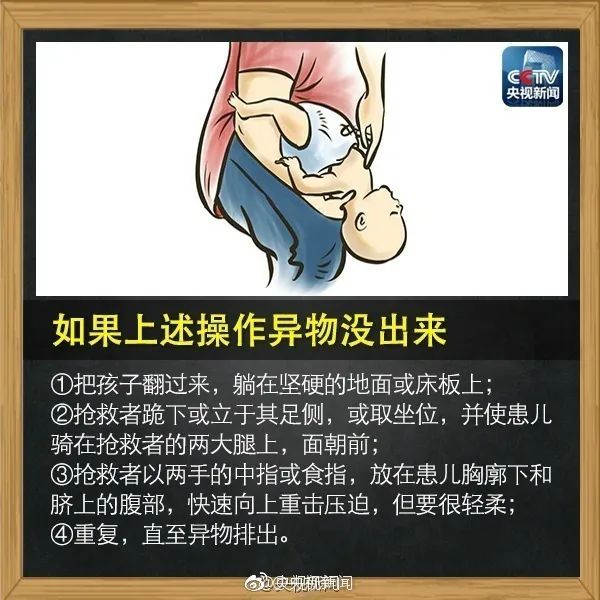
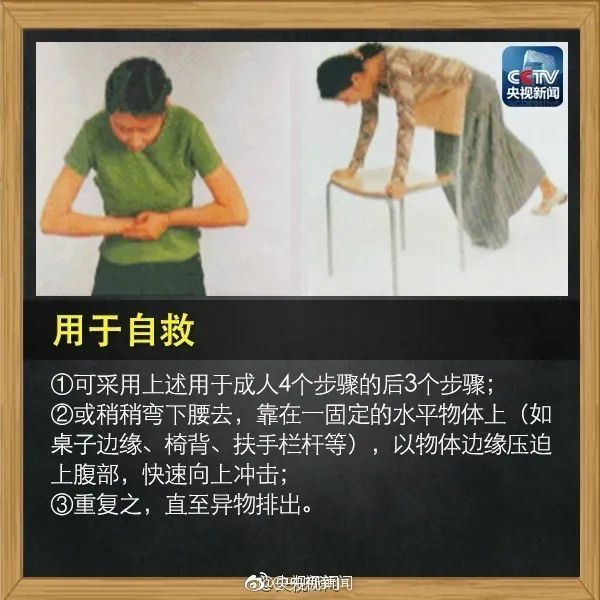
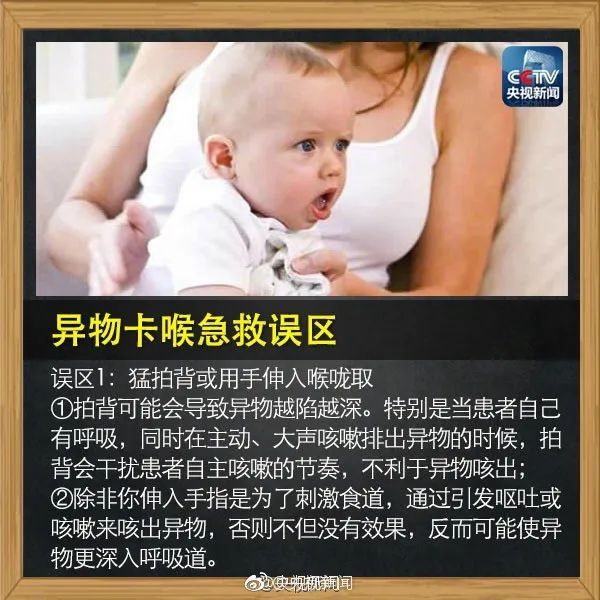
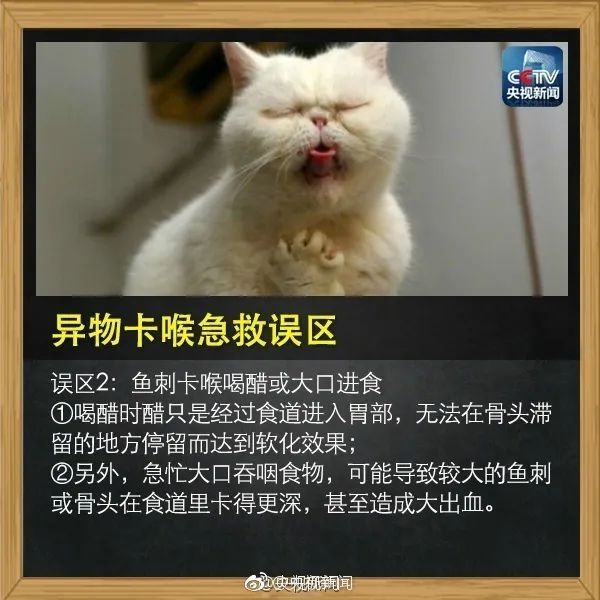
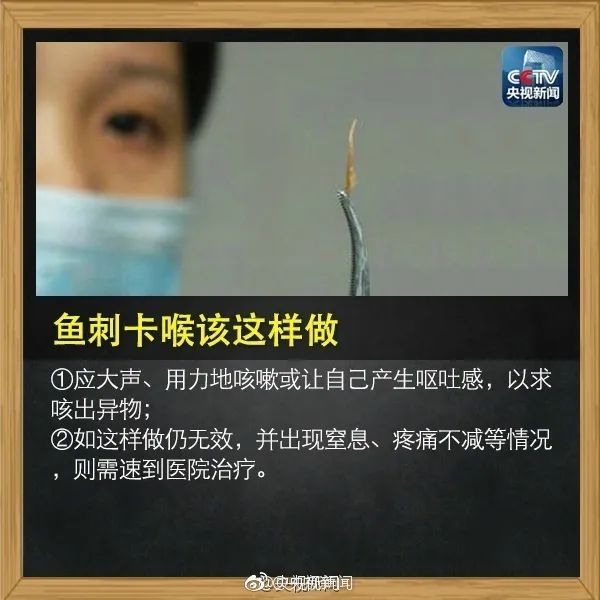
What should I do if food accidentally enters the trachea?
Remember this Heimlich maneuver!
Critical moments can save lives
 < /p>
< /p>

Source: Comprehensive Nanguojin Reporter Wei Li@CCTV News, Modern Express, Sanjiang Metropolis Daily, etc.