The knee joint is one of the most complex joints in our body. It is composed of the articular surface of the lower end of the femur, the articular surface of the upper end of the tibia and the articular surface of the patella, which are wrapped by the joint capsule, and play a linking role in the kinematic chain of the entire lower limb.
Sun Chao, a therapist from the Rehabilitation Department of Shandong Provincial Hospital of Traditional Chinese Medicine, introduced that after a stroke, due to the decreased neuromuscular control of the patient and the destruction of the stability of the knee joint, many patients will experience knee hyperextension or hyperextension. The phenomenon of knee collapse. Knee hyperextension, also known clinically as opistonia or retroflexion deformity, refers to the hyperextension of the femoro-tibial joint in the sagittal plane (knee extension angle) during the stance phase of the affected lower limb during the gait cycle. >5°). If the knee hyperextension is not corrected in time, it will cause repeated damage to the knee joint. Over time, it will destroy the articular cartilage, the joint capsule and ligaments at the back of the knee joint, resulting in irreversible chronic knee joint disease.
Sun Chao said that at present, the reasons for knee instability in patients after stroke are not very clear. Common causes include: abnormal muscle function, abnormal range of motion, and lower limb proprioception disorders. Knee instability is caused by a combination of factors, which not only affects the patient’s walking ability, but also brings irreversible joint disease to the patient. It is of great significance to detect and correct this complication in a timely and effective manner.
1. Proprioceptive training: Proprioception plays a vital role in maintaining joint dynamic stability, inducing normal movement, and preventing joints from external injury.
2. Quadriceps muscle strength and endurance training: use the quadriceps femoris isokinetic trainer.
3. Supine position knee extension control: instruct the patient to take the supine position, perform 0-15° knee flexion training and keep the posture at 15° for 10 s, during which the ankle joint is kept in a neutral position to prevent foot Inverted.
4. Progressive knee flexion training in prone position: the patient is in prone position, and the patient is instructed to practice knee flexion training under the condition of resistance. Start at the angle and gradually increase the degree. Note that the torso is not tilted, and there is no waist and hip compensation.

5. Seated knee flexion ball training: the patient sits upright on the treatment table, with the edge of the bed in the middle of the thigh. Put a soccer ball on the foot of the lower extremity on the affected side, put the affected foot on the soccer ball, and let the patient practice rolling the ball with the knees bent in four directions, front, back, left, and right. Pay attention to keep the torso in a neutral position, do not tilt, and roll the ball slowly and steadily.

6. Control training for ascending and descending stairs: The therapist stands behind the patient and uses the knee joint to touch the popliteal fossa of the affected limb to make the affected leg Stand with weight and keep knees flexed at 0° to 15°, and perform 20 times up and down the stairs with the healthy leg. Pay attention to prevent excessive flexion of the hip joint.

7. Assisted walking training: The therapist uses one hand or knee joint to touch the patient’s popliteal fossa to prevent the knee from hyperextension when walking, and the other hand to touch the patient’s knee. The patient circles the upper edge of the pelvis on the affected side to prevent him from walking.
8. Semi-squat training: The therapist guides and assists the patient to stand in front of the corrective mirror with feet apart (shoulder-width apart), instruct the patient to squat, and make the affected limb when squatting. Fully loaded, half squat for 45 s/reps, starting at 0° and ending at 60°.
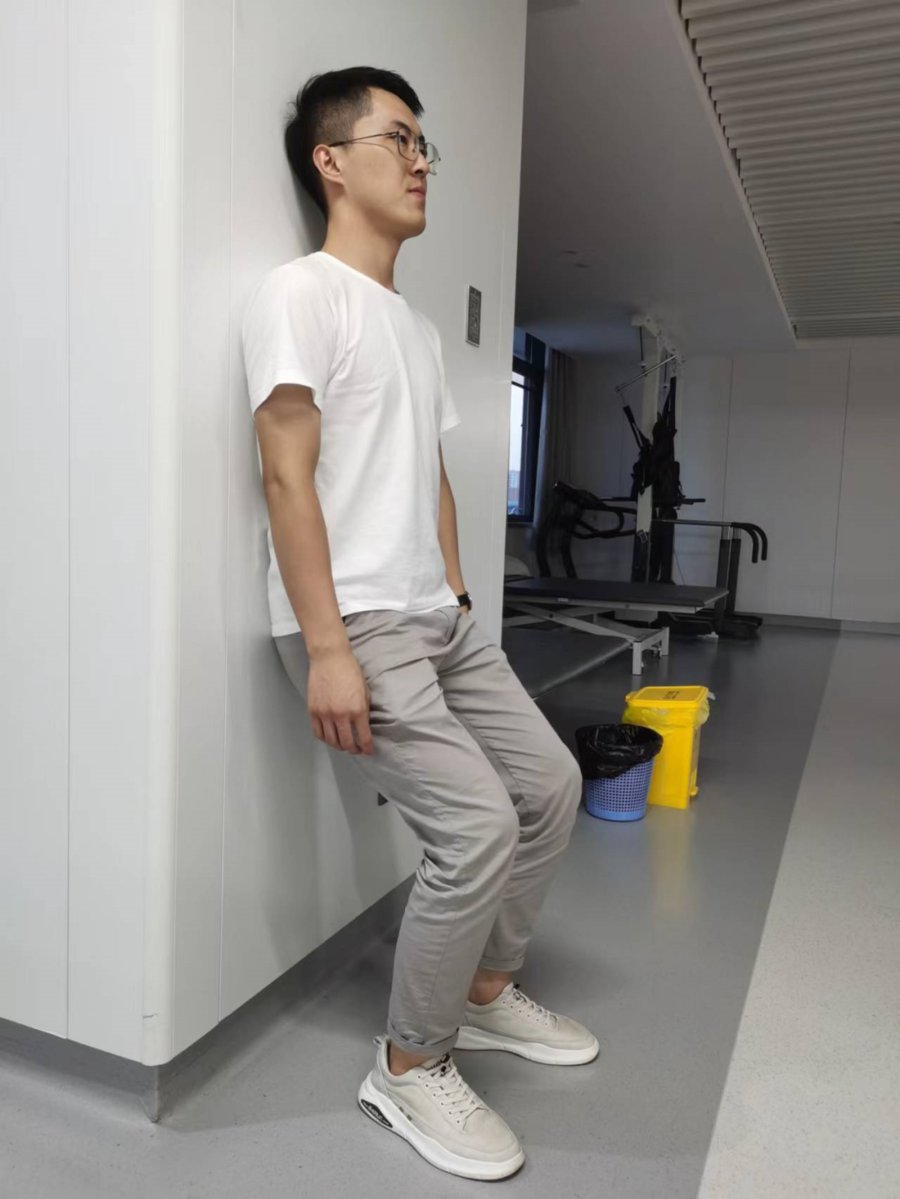
9. Bobath facilitation training: the patient is standing, leaning against the wall, and a Pilates ball is placed behind the knee joint of the patient’s lower extremity. The teacher sits on the knees in front of the patient, with the base of the palms on the quadriceps muscle, and promotes from the proximal end to the distal end to increase sensory input and establish a correct body diagram. Then have the patient slowly control the extension and flexion of the knee. Pay attention to increase the appropriate number of exercises according to the patient’s physical strength.

10. Lower extremity training for knee hyperextension with PNF technique: the patient is in a supine position, the therapist holds the patient’s ankle joint with one hand and the other hand on the patient’s popliteal Immobilize the patient’s thigh above the socket. The patient is instructed to bend the knee, use the isotonic combination technique, first perform a concentric motion of knee flexion, the therapist applies resistance, and then perform an eccentric motion when the joint ends, and instruct the patient to continue to maintain the direction of the strength of the knee flexion, the password: “Continue to maintain Bend your knees and let me slowly pull you.” The therapist straightens the patient’s knee joint hard. Since then, the hamstrings first complete the concentric movement and then the eccentric movement. This process is called isotonic combination. Be careful not to lean your body, control the amount of training according to the patient’s condition, and don’t be overly fatigued.