內容目錄
He Lin, Deputy Chief Physician, Department of Respiratory and Critical Care Medicine, Fuling Hospital Affiliated to Chongqing University
Xiao Lin is a 17-year-old middle school student, a flowery girl. Unexplained cough, wheezing, intermittent phlegm and blood for 2 months, was diagnosed as asthma many times, but the treatment was ineffective, and the condition was progressive. On May 9, 2022, he came to our outpatient department of thoracic surgery for dyspnea. A chest CT scan revealed a mid-tracheal mass that almost completely obstructed the trachea. Therefore, she was admitted to the thoracic surgery hospital.
House leakage happens to rain overnight, and the severe winter in October will make it worse.
For the tumor that almost completely blocks the trachea, it must be removed as soon as possible. However, which surgical method to adopt and how to reduce the risk of anesthesia and surgery need to be carefully studied. At 9:00 a.m. on May 10, 2022, while the doctors were still discussing how to choose a surgical plan, Kobayashi’s breathing difficulties further aggravated. He could not lie down, but could only breathe in a sitting position. His lips were cyanotic, and his heart rate reached 160 beats/min. Intermittent hemoptysis occurs. Kobayashi’s face was full of anxiety and panic, his chapped lips and eager eyes stimulated the nerves of every medical worker. In order to further clarify the nature of the lesions and formulate a better surgical plan, enhanced CT and three-dimensional reconstruction were performed again.
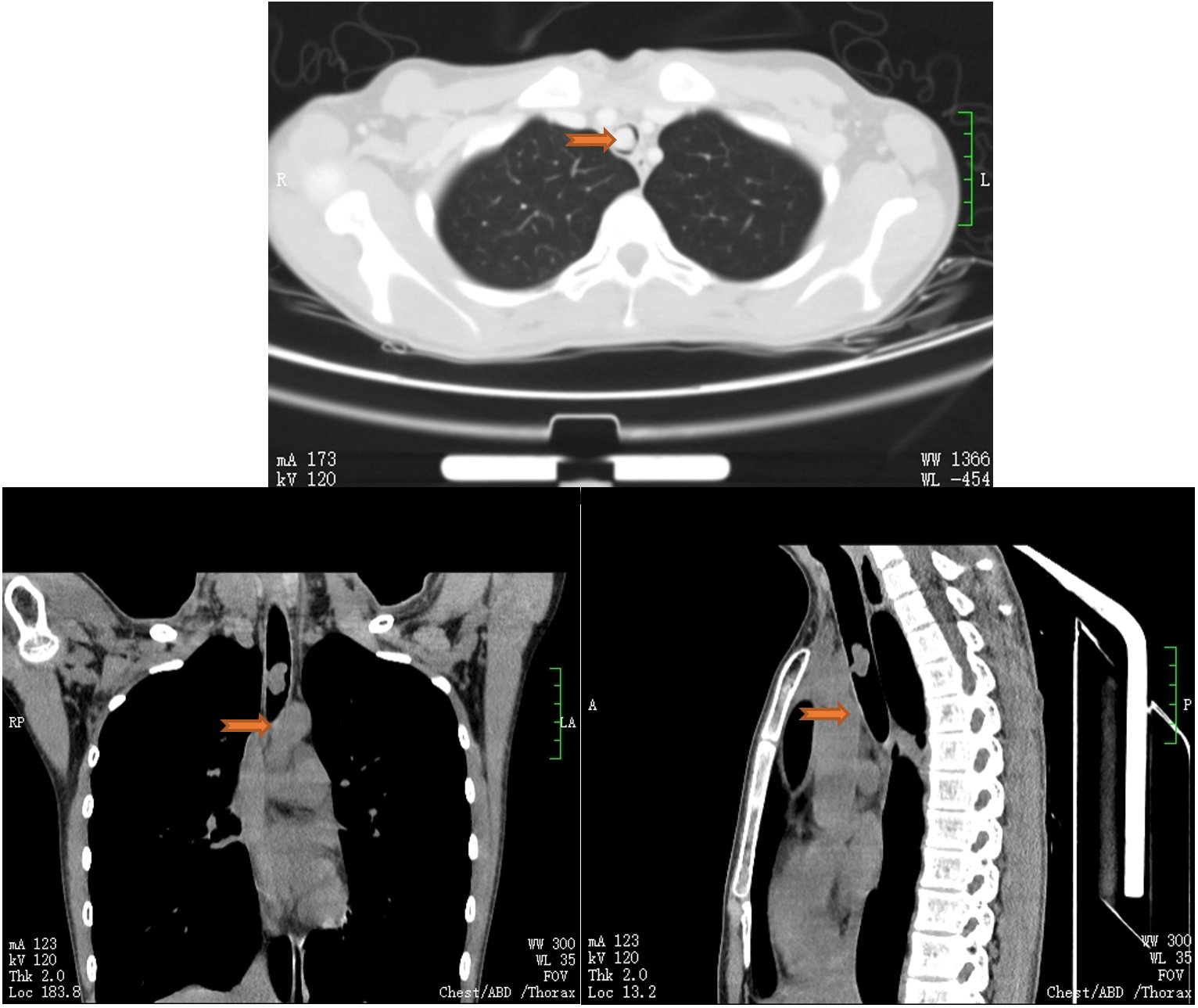
Emergency chest CT showed that the tumor was in the middle of the trachea, blocking about 90% of the airway. The enhanced CT showed that the CT value of the tumor was 209hu, which was close to the CT value of the intravascular contrast agent, indicating that the blood supply was extremely rich, and there was a possibility of tumor rupture and hemorrhage during the operation. In addition, hemoptysis has occurred, and high fever (the highest temperature is 39.5 ℃) has also appeared. CT shows that the lung infection lesions have also increased significantly. Makes the already difficult operation even more dangerous. How to implement anesthesia for surgery when the airway is almost completely blocked? What about bleeding? What to do if the tumor ruptures? The difficulty of surgical implementation has exceeded the ability of conventional single-disciplinary treatment.

Multi-disciplinary collaboration to provide good strategies, breathing intervention to provide good recipes
Life is the first, we must do our best All ability to heal. Due to the critical condition of the patient, the operation is difficult and the risk is high. At 1:00 noon on May 10, 2022, under the auspices of the Medical Department, the patient had an emergency MDT consultation. The MDT was composed of experts from the Department of Respiratory and Critical Care Medicine, Thoracic Surgery, Department of Anesthesiology, Department of Radiology, and ICU. The discussion team, Chief Physician Liao Xiuqing of the Department of Respiratory and Critical Care Medicine, led the backbone of the intervention team in the department, Deputy Chief Physician He Lin, Chief Physician Tao Tao and Chief Resident Wang Ling, and participated in the discussion as a specialist team.
In the discussion, everyone agreed that the patient may be a benign tumor, and the possibility of cavernous capillary hemangioma is high. Due to the severe airway obstruction and abundant blood supply by the tumor, there is a high risk of hemorrhage and suffocation after rupture. At the same time, surgery requires thoracotomy to remove a section of the diseased trachea, which is not only risky but also costly for a benign tumor. Therefore, everyone finally reached a unified opinion: airway interventional therapy should be the preferred treatment plan, and the thoracic surgery department, anesthesiology department, and ICU should be fully prepared for surgery at any time due to tumor rupture and massive hemorrhage. The specific surgical plan is as follows:
1. Preoperative blood preparation, tracheal intubation, ventilator, CPR drugs and instruments, hemostatic drugs, etc. are prepared.
2. Intraoperative tracheal intubation was inserted 2cm above the tracheal tumor, and then a high-frequency electrical snare was introduced through a bronchoscope to cover the root of the tumor to remove the tumor. If the tumor ruptures and bleeds heavily, the tracheal intubation tube should be inserted forward immediately, the balloon of the tracheal intubation tube should be used to cover and compress the airway at the bleeding site of the tumor root to compress the hemostasis, and the resected tumor should be pushed into the left or right main bronchus with a bronchoscope. In this way, unilateral lung ventilation is ensured, and then the patient is transported to the operating room for surgery while the blood volume is replenished and the vital signs are maintained relatively stable.

Preoperative communication and anxiety, careful operation is guaranteed
This operation is difficult and high-risk , the patient has the possibility of directly dying on the operating table. The patient’s family fully understood the urgency, necessity and risks of the operation through the patient’s explanation of the preoperative preparation and operation plan, especially the safety measures of multidisciplinary cooperation, and did not choose hospital transfer or surgery, but chose Airway intervention, ready for surgery.
The disease was cured, and the operation was successful, and the airway was smooth
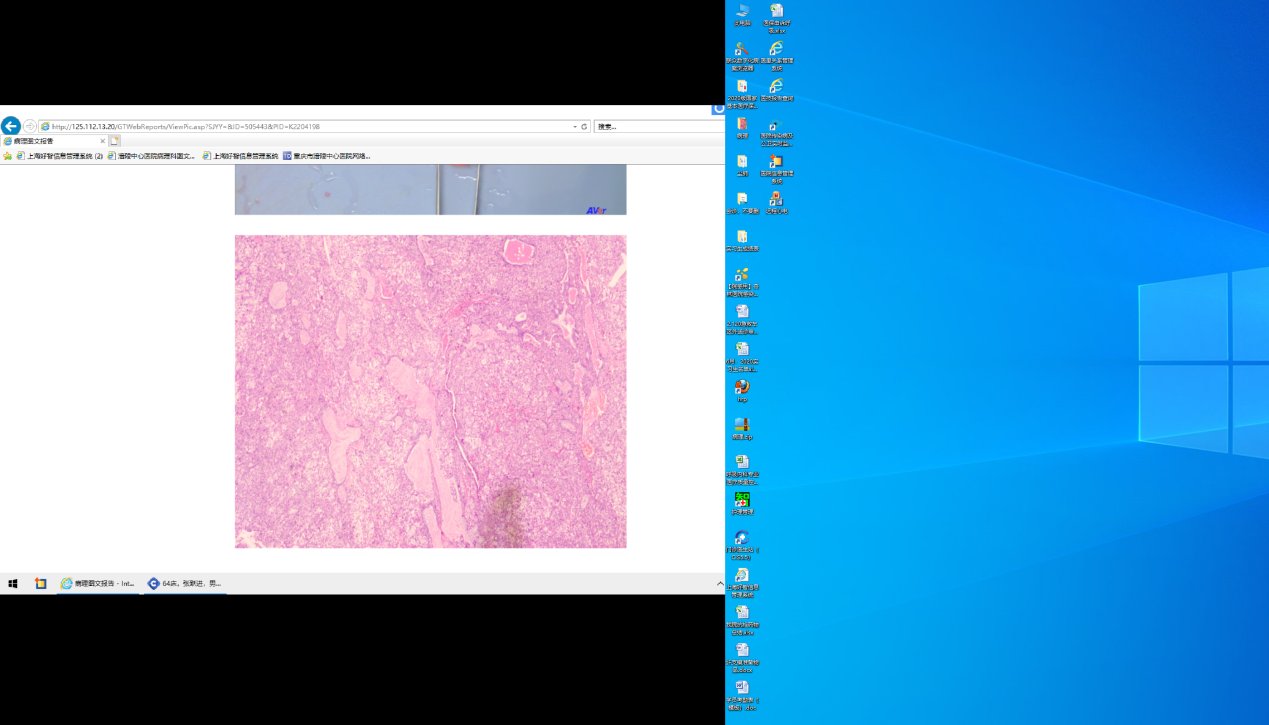
On the one hand, there was severe breathing difficulty and suffering, on the other hand, the fear of surgery, Xiao Lin was sent to the intervention room with an extremely nervous mood . Deputy Chief Physician He Lin first conducted psychological counseling for Xiaolin to relieve tension, and then connected to a non-invasive ventilator to improve the patient’s dyspnea. With everyone’s encouragement and the effect of sedatives, Xiaolin quickly entered the operation state quietly. The operation was personally guided by Chief Physician Liao Xiuqing and performed by Deputy Chief Physician He Lin. When the bronchoscope entered the airway, it was found that the tumor almost completely blocked the lumen, and the surface of the trachea and tumor was covered with blood. Through gentle and meticulous operation, it was seen that the tumor grew out of the trachea wall, and the tumor moved up and down with breathing, and the tumor was partially recovered. There is active bleeding.
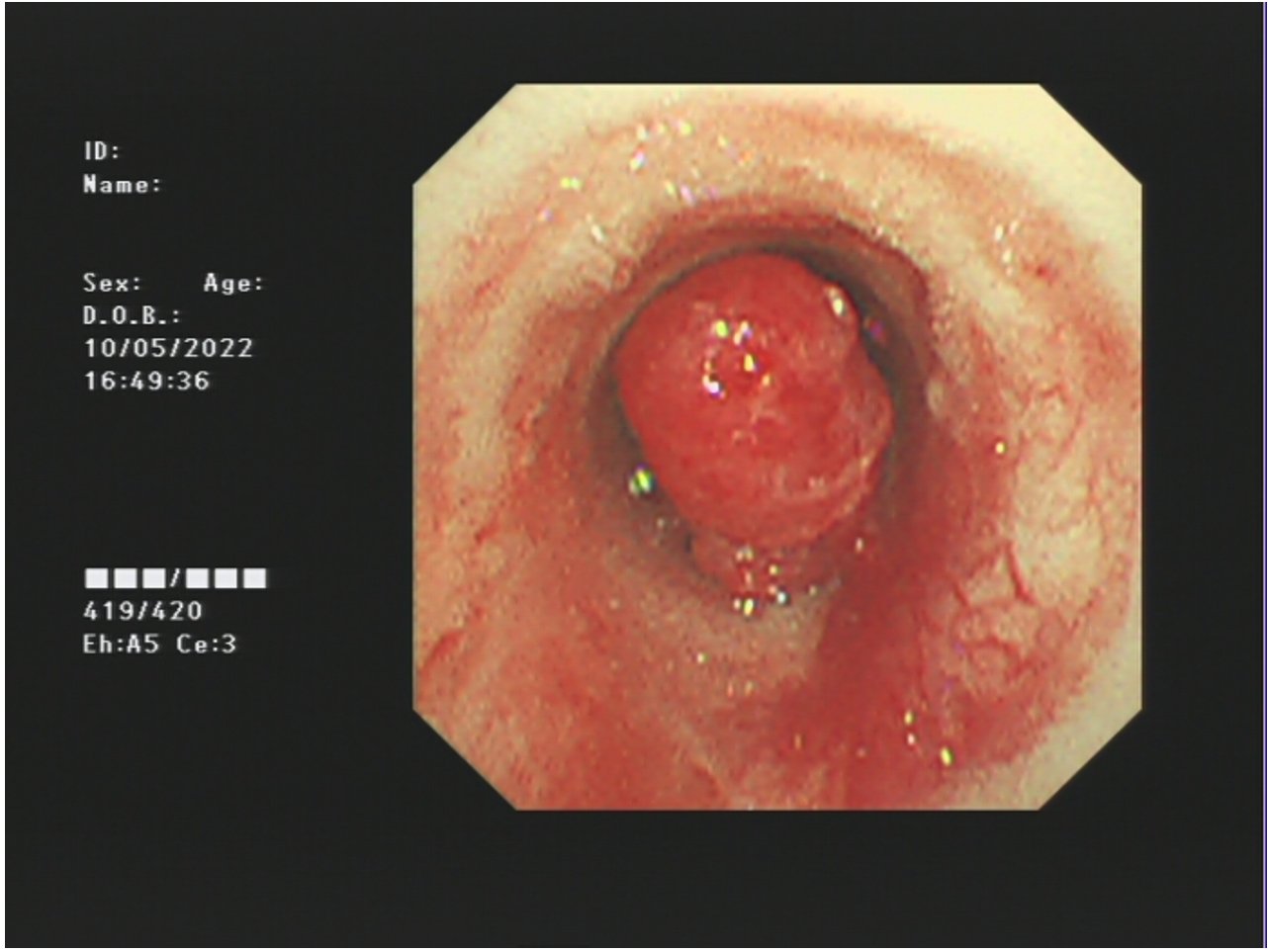
New creatures in the middle of the trachea, rich blood supply, local bleeding
Fully understand the situation in the airway , In the face of various risk factors such as suffocation and bleeding, the team once again made detailed and prudent surgical strategies to try their best to ensure the success of the surgery and reduce the occurrence of risks. Endotracheal intubation, electric snare, argon knife treatment, cryotherapy… After 1 hour of intensive and orderly surgical treatment, the tumor was completely excised, and the bleeding was well controlled.

tumor removal
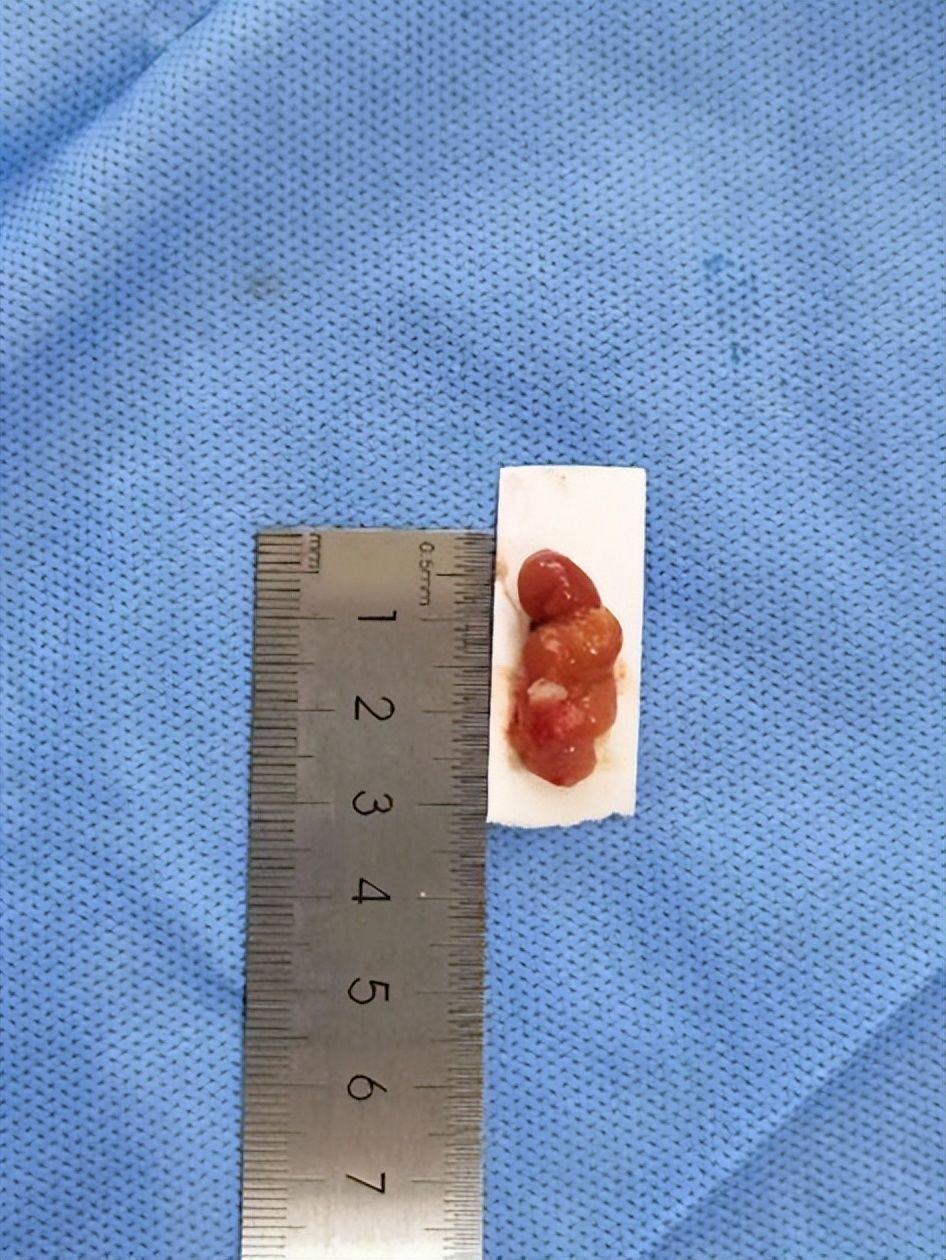
Take out the tumor tissue (30mm*10mm)
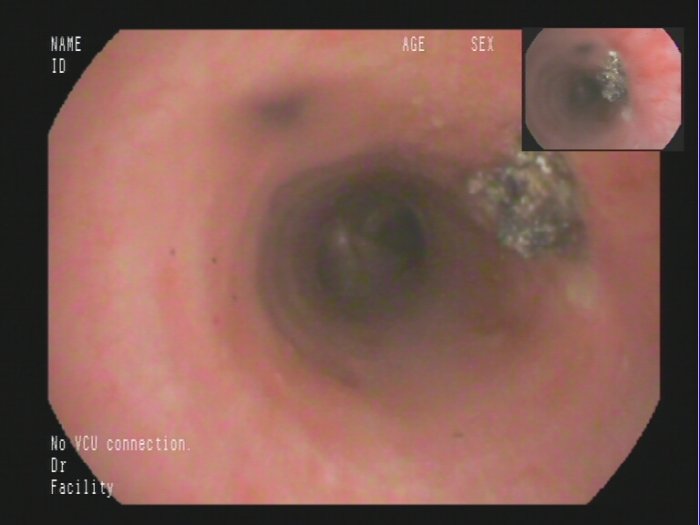
Postoperative airway
Postoperative airway
Seeing that the bright red tumor was taken out, the trachea that was originally blocked was restored, and the operation was a complete success. Xiaolin gradually woke up, everyone’s hearts were restored to calm, and more was the joy of success .Seeing Xiaolin being quietly pushed out of the operating room, the parents’ eyes are full of grateful tears and long-lost smiles.
The danger is finally safe. Thanks to the active efforts of the team, the Kobayashi operation has been successfully performed, symptoms such as dyspnea, fever, and hemoptysis have been significantly relieved, and the bronchoscopy lesions have been significantly improved. The possibility of glandular tumors is high. Since this type of tumor is rare in clinic, in order to ensure the accuracy of diagnosis and guide the next treatment, the pathological specimens have been sent to the Department of Pathology, Southwest Hospital for further diagnosis.
Post-Electrical Snare Treatment
neoplastic lesions, low-grade mucoepidermoid carcinoma?

Post-Electrical Snare Treatment
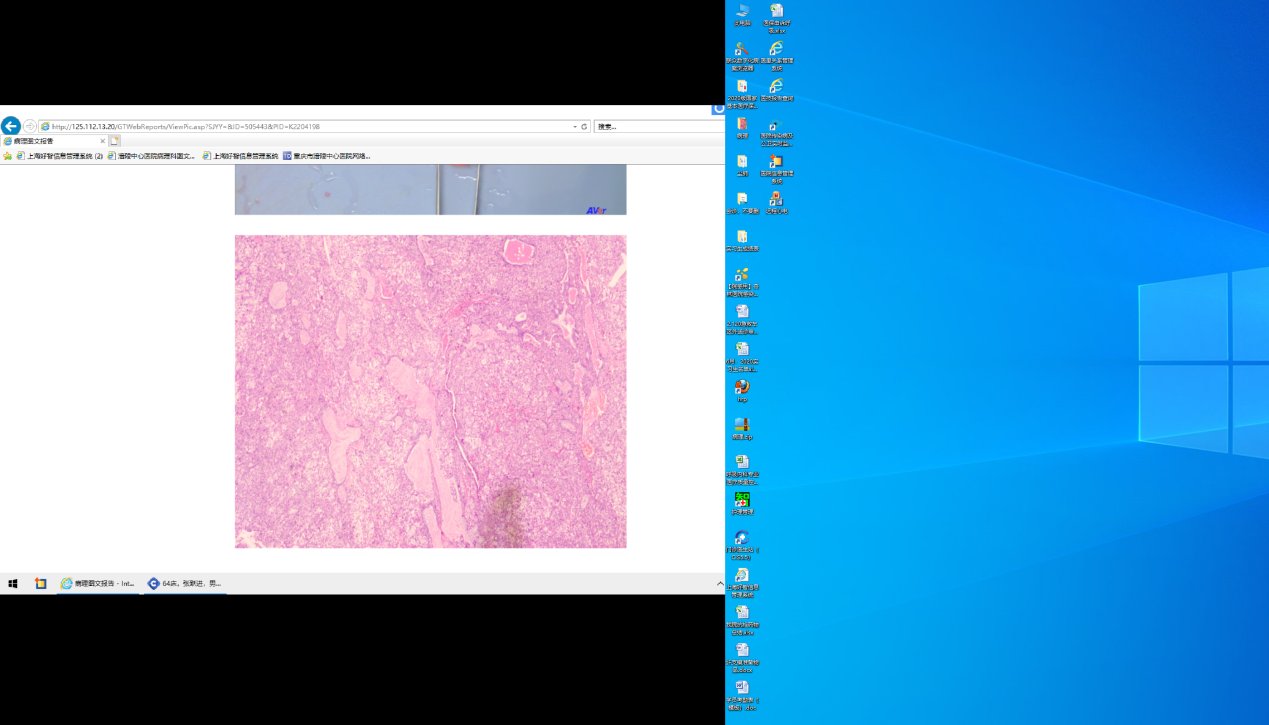
neoplastic lesions, low-grade mucoepidermoid carcinoma?