
△ Example of a restrictive scar caused by a straight incision on the flexor surface of a finger
/////////
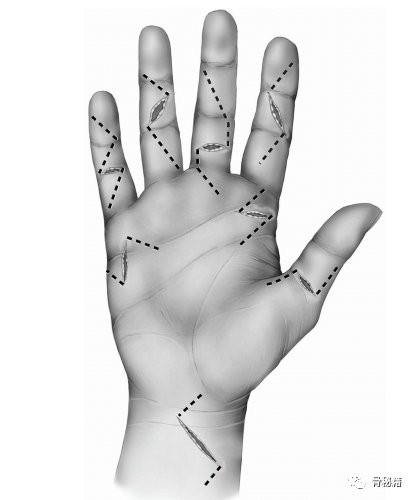
< p> Due to the complexity of hand and wrist functions, the incision in this area is unique. Proper planning of the incision is important to ensure healing and maintain function. The finger has a well-established approach to good exposure of deeper structures without compromising healing. Improperly positioned incisions can result in restrictive scarring, which may result in reduced movement and function. In addition, limited skin redundancy on the palmar surface may make delayed closure of edematous wounds difficult. Proper planning of hand and wrist incisions will help avoid some of these difficulties.
Fingers
There are several common methods of treating the volar side of the fingers and thumb. The traditional Bruner incision is the most common method. It is a zigzag incision angled at the flexion creases of the metacarpophalangeal (MP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints. The flexion crease of the palm is also a point of change in orientation as the incision is advanced proximally. The principle is based on the fact that longitudinal incisions across these creases create excessive scarring and limit extension. For optimal flap healing, it is best to keep the angle around 90 degrees. Sharper angles than 60 degrees result in a higher incidence of skin necrosis.

A: Bruner incision method on the palm of the finger. The most common method of cross-buckling creases is to use these wavy, oblique cuts. B: Excellent exposure to the palm side of the fingers can be achieved.
C: These scars usually heal well.
An alternative to Bruner’s incision in the finger is the medial-lateral approach. It has the advantage of being more cosmetically attractive. The incision is made on the outside (or inside) of the finger, and the skin is elevated to expose the underlying tissue. A good way to ensure that the surgeon is not directly over the neurovascular bundle is to connect the incision at the apex of the flexion crease. This is also the method of choice for replantation surgery. While cosmetically appealing, the challenges of this technology include lifting the skin and ensuring its vitality.
In cases of flexion deformities of the fingers, such as Dupuytren’s contracture, a straight midline incision with Z-plasty is an alternative to the traditional Bruner incision. This will allow the incision to be lengthened while correcting the flexion deformity. The 60-degree angle helps keep the flap tip alive.
Dorsal Finger Incision
The dorsal skin of the hand lacks rough connections and has more redundancy due to joint flexion requirements. Due to this redundancy, longitudinal cuts are acceptable. Longitudinal incisions allow preservation of venous and lymphatic drainage while providing good exposure of the extensor mechanisms. Inert S or curved cuts can also be designed to avoid cross extending creases. The incision at the distal interphalangeal joint can also be longitudinal, but dissection may be limited due to the nail bed and distal folds. Another option is a “T” or “H” shaped incision that allows visibility of the extensor mechanism and the distal interphalangeal joint.
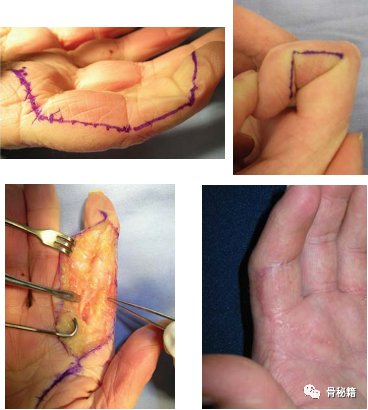
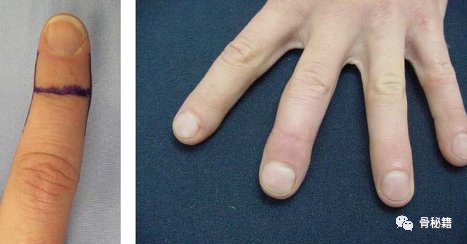
A: Mid-axis or lateral approach of the finger. This technique can be more aesthetically pleasing than a Bruner incision.
B: Care must be taken to connect the incision at the apex of the flexion crease to avoid direct dissection of the underlying neurovascular structures and to prevent excessive volar scarring.
C: Although more dissection is required, excellent exposure can be achieved.
D: An example of a healed medial-lateral incision.
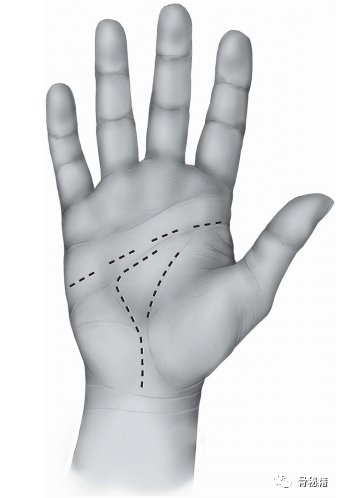
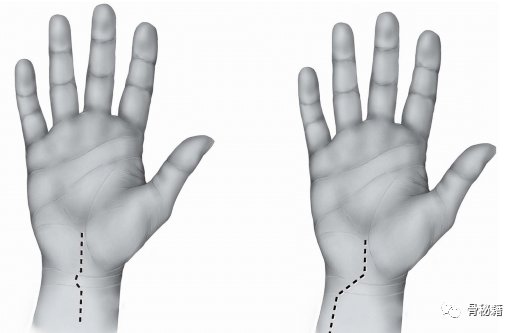
volar incision of the hand
A transverse incision or incision parallel to the flexion crease provides the best cosmetic result. However, these incisions are perpendicular to the underlying blood vessels, nerves, and tendons. Therefore, care must be taken when implementing these methods. A transverse incision consistent with the metacarpophalangeal joint flexion crease has been found to produce better esthetic results and less restrictive scarring at the base of the thumb for A1 pulley release. The traditional longitudinal Bruner-type incision is commonly used and is useful when more exposure is required. Again, follow the basic premise of changing direction at the crease to minimize scarring. A wound or scar is at risk of developing a function-limiting scar. Depending on the patient, these may sometimes require revision z-plasty. Palmar incision of the hand.

A: Longitudinal z-plasty approach on the volar side of the finger in the presence of pre-existing flexion contractures such as Dupuytren’s contracture Very useful.
B: Easy wound closure with little or no tension at full finger extension.
A: An “H”-shaped incision on the dorsal side of the distal interphalangeal (DIP) joint provides a good Dorsal side of side fingers. B: The wound usually heals well.

△ Two common approaches for the back of the fingers: a straight portrait and a more curved portrait to avoid stretch creases.
When exposing the carpal tunnel, a longitudinal incision is usually used, preferably in or in line with the palm line. To extend the incision proximally, a Bruner-type zigzag incision can be made between the distal and proximal flexion creases of the wrist. These angled cuts are the most common and common occurrence of crossed hand and wrist flexion creasesmethod used. Care should be taken to maintain the ulnar to the palmar longus tendon to avoid injury to the volar sensory branch of the median nerve.
Longitudinal incision without risk of restrictive scarring. Lateral and curvilinear cuts can also be used on the hands if desired. The skin on the hand is movable and scarring is usually not a functional problem as the flexor tendons are the main force and will minimize functional deficits. Approaches to the carpometacarpal joint can be performed longitudinally between the abductor pollicis longus and extensor pollicis brevis tendons, or they can extend laterally proximally along the wrist flexion crease.

Cut using the trigger finger method of the palm bend crease.
These result in an aesthetically pleasing scar with little or no residual imperfections.
The longitudinal Bruner-type incision is preferred when greater exposure is required.
Surgical incisions and skin lacerations
Flexor tendon lacerations Skin lacerations are very common clinical conditions. In these cases, the previously mentioned surgical approach must be modified to incorporate skin lacerations. As a general rule, the Brunner zigzag approach can be used to extend the skin laceration proximally or distally. Adequate surgical exposure is required to identify and expose the tendon ends. A torn flexor tendon is often retracted in the palm unless an intact tie or psoas prevents further proximal retraction. The proximal end of the tendon may be retracted so much that extensive exposure is required. Another option is to perform a separate proximal surgical exposure and retract the tendon at this point and retract it into a more distal surgical approach under the intact skin bridge. Such incisions can be made at the level of the palm crease distal to the palm. In the case of an FPL laceration at the base of the thumb, the proximal portion of the tendon usually contracts beneath the thenar musculature and even into the palm.
Skin wounds should be closed as soon as possible, but not necessarily immediately, to reduce the chance of wound infection. Immediate coverage is essential whenever tendon, bone, or neurovascular structures are exposed. It is preferable if primary skin closure can be achieved without tension; otherwise, some type of skin grafting is best.
△ Skin laceration and incision to explore tendon.
Here are some common cutouts

Disclaimer: The content and pictures in this article are reproduced content. If there are copyright issues, please contact us in time. We will deal with it immediately and take protective measures to protect the interests of both parties.
Why submit? Is to record their own medical path! It is to communicate and share with more orthopedic colleagues! It is for more people to see and benefit! Making the dissemination of knowledge a habit is the reason why “Jiujiu Orthopedics” let you contribute!